Dexamethasone: the cheap, old and boring drug that's a potential coronavirus treatment
- Written by Nial Wheate, Associate Professor | Program Director, Undergraduate Pharmacy, University of Sydney
First, we tried the antimalarial drug hydroxychloroquine. Then we tested the antiviral drug remdesivir. But new UK research gives the strongest indication yet we may have found a useful treatment for COVID-19.
This time it’s an old anti-inflammatory drug, dexamethasone, which has been described as cheap, old and boring.
Preliminary results from a clinical trial just released indicate the drug seems to reduce your chance of dying from COVID-19 if you’re in hospital and need oxygen or a machine to help you breathe.
The results were significant enough for the UK to recommend its use for severe COVID-19.
Before we roll it out in Australia, we need to balance the drug’s risks with its benefits after peer-review of the full trial data.
What is dexamethasone?
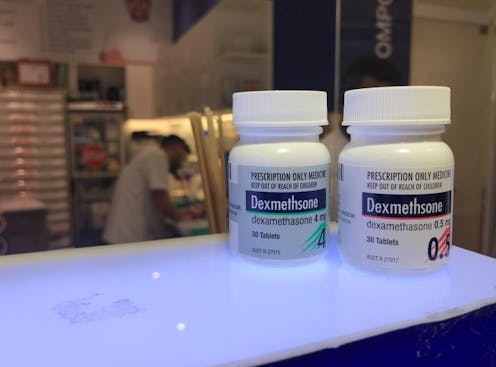
Dexamethasone has been used since the late 1950s, so doctors are familiar with it. It’s also inexpensive, with a packet of 30 tablets costing around A$22 (for general patients) under Australia’s Pharmaceutical Benefits Scheme.
So if it does work for COVID-19, this cheap and boring drug, already available in Australia with a prescription, would be easy to add to current treatments.
Dexamethasone belongs to a class of drugs known as corticosteroids and is used to treat a range of conditions related to inflammation. These include severe allergies, some types of nausea and vomiting, arthritis, swelling of the brain and spinal cord, severe asthma, and for breathing difficulties in newborn babies.
And it’s dexamethasone’s application to those latter two respiratory conditions that prompted doctors to think it may also help patients severely affected by COVID-19.
Read more: ICU ventilators: what they are, how they work and why it's hard to make more
What did the trial find?
The recently reported results come from the Randomised Evaluation of COVID-19 Therapy, or RECOVERY, trial.
The researchers put patients into one of three groups: those needing ventilation (a machine that helps them breath); those who just needed oxygen therapy; and those who needed no treatment to help them breathe.
Patients in each of those groups were given dexamethasone (6mg once a day, either as a tablet or via intravenous injection), for ten days. A fourth group (a control group) was not given the drug.
Dexamethasone was most useful for the ventilated patients; deaths for this group dropped by about one-third with drug treatment. In contrast, deaths only dropped by one-fifth for those patients who were only receiving oxygen therapy. There was no benefit to patients who could breathe normally.
Results of the dexamethasone trial have just been released.The researchers calculated that giving dexamethasone to eight ventilated patients would prevent one from dying, on average. And giving it to around 25 patients needing oxygen alone would prevent one death.
Read more: The fascinating history of clinical trials
How might dexamethasone work for COVID-19?
When a patient has severe COVID-19, their immune system ramps up to catch and control the virus in the lungs.
In doing this, their body produces more infection-fighting white blood cells. This results in inflammation and pressure on their lungs, making it very difficult for them to breath.
It’s therefore likely dexamethasone reduces this inflammation, and so reduces pressure on the lungs.
Read more: How does coronavirus kill?
What are the downsides?
There are potential complications with using dexamethasone.
First, dexamethasone also suppresses the immune system when it reduces inflammation. So, it’s not usually recommended for people who are sick, or could be sick, from other infections. So doctors will need to make sure patients have no other infections before they are prescribed the drug.
If the results of this trial are correct though, the drug doesn’t appear to compromise the patient’s ability to fight COVID-19; it might just affect their ability to fight off other diseases.
Second, the drug is only useful for patients with difficulty breathing and needing some assistance either through ventilation in a hospital or from oxygen therapy.
There appears to be no benefit for patients who don’t need help breathing. So we shouldn’t be giving it to everyone who tests positive to the virus.
Third, like all drugs, dexamethasone has side effects that need to be monitored. Serious, but rare ones include: severe stomach or intestinal pain, sudden changes with vision, fits, significant psychiatric or personality changes, severe dizziness, fainting, weakness and chest pain or irregular heartbeat, and swelling of the face, lips, mouth, tongue or throat, which may cause difficulty in swallowing or breathing.
What happens next?
The results of the clinical trial are preliminary. So we need to wait for the full study data and scientific peer-review before we can make a definitive decision as to whether dexamethasone treatment is a worthwhile, and safe, addition to COVID-19 therapy in Australia.

